About Pediatric Food Allergies
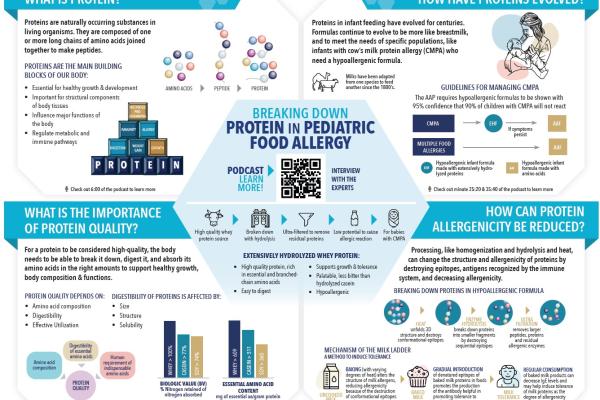
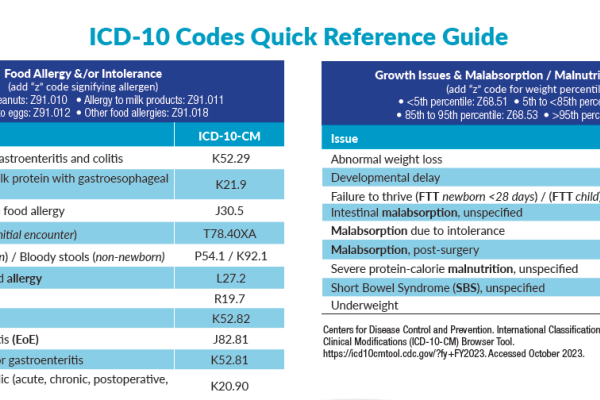
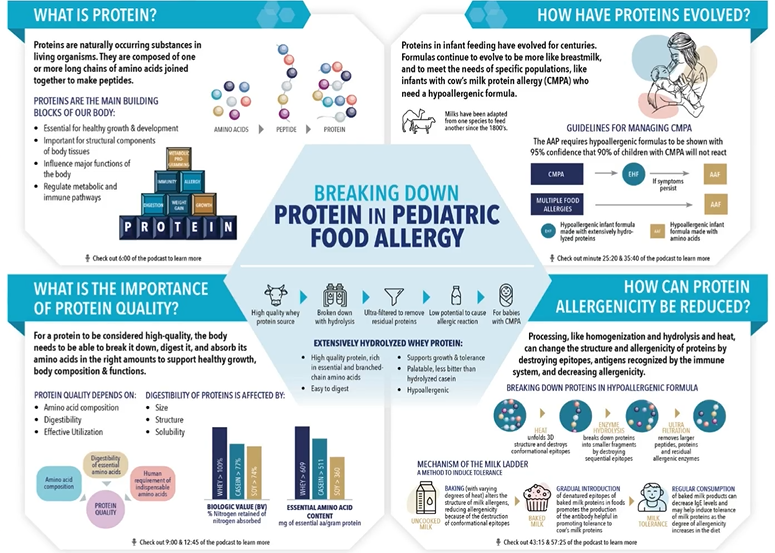
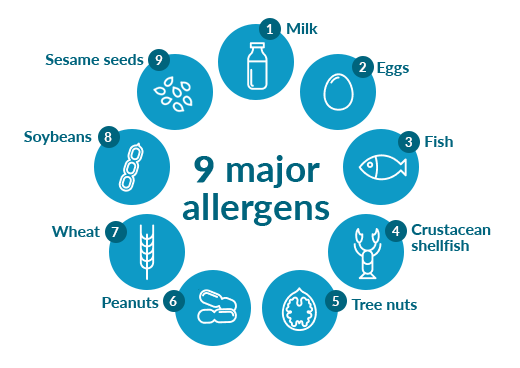
Food allergy is defined as an immunologic response or reaction to the ingestion of food that involves an immune-mediated response, which leads to signs and symptoms of an allergic disease. There are some foods to which children are most frequently allergic to, such as cow's milk, soy, wheat, eggs, peanuts, tree nuts, shellfish, and sesame seeds.
Pediatric food allergies are on the rise, are most common early in life, and often present with diverse and non-specific symptoms, making them challenging to diagnose and manage.
At Nestlé Health Science, we understand this challenge and are committed to supporting healthcare professionals, patients and caregivers in caring for infants and young children with food allergies, such as cow's milk protein allergy (CMPA), eosinophilic esophagitis (EoE), food protein enterocolitis syndrome (FPIES), and intolerances.
The most prevalent food allergy in infants and children 0-2 years of age is cow's milk protein allergy (CMPA). It occurs when an infant’s immune system reacts abnormally to the proteins in cow’s milk, which are either transferred from the mother while breastfeeding or from cow’s milk protein-containing formulas and complementary food. The immune reaction may be immunoglobulin (Ig)E-mediated, non-IgE-mediated, or mixed. The reactions can be immediate (early) reactions, occurring from minutes to hours after exposure, and/or delayed (late) reactions, which can manifest 48 hours or even a week following ingestion. Immediate reactions are more likely to involve IgE, but combinations of immediate and delayed reactions can occur in some infants. Regardless of whether a food allergy is IgE mediated, non-IgE mediated, or both, the dietary management of a food allergy is avoidance of the offending food allergen.1
Symptoms of CMPA can occur in the digestive tract, on the skin, in the respiratory tract, or in other general areas. Some symptoms include vomiting, diarrhea, blood in the stool, eczema, runny nose, wheezing, anaphylaxis or failure to thrive.
Early detection and appropriate intervention is essential to minimize the impact of CMPA in infants and children. CMPA can be difficult to diagnose given the large variability in number and severity of the symptoms, and the fact that some of them are perfectly normal for infants to experience. In addition, when CMPA is suspected or diagnosed, infants should be placed on an elimination diet that is free of cow's milk protein.
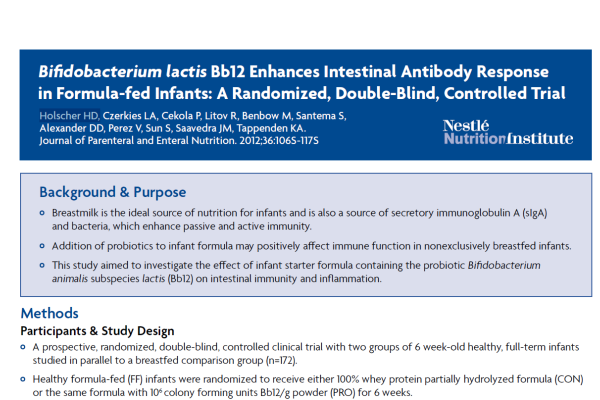
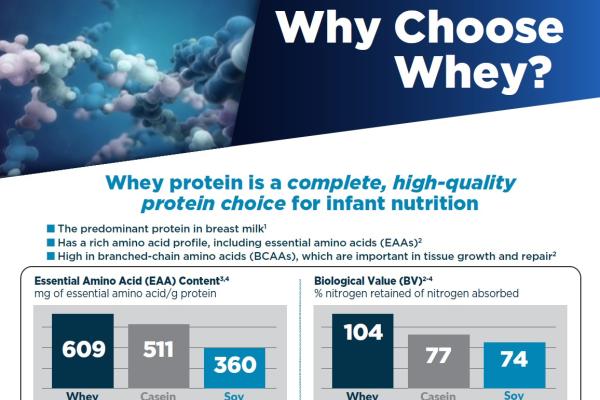
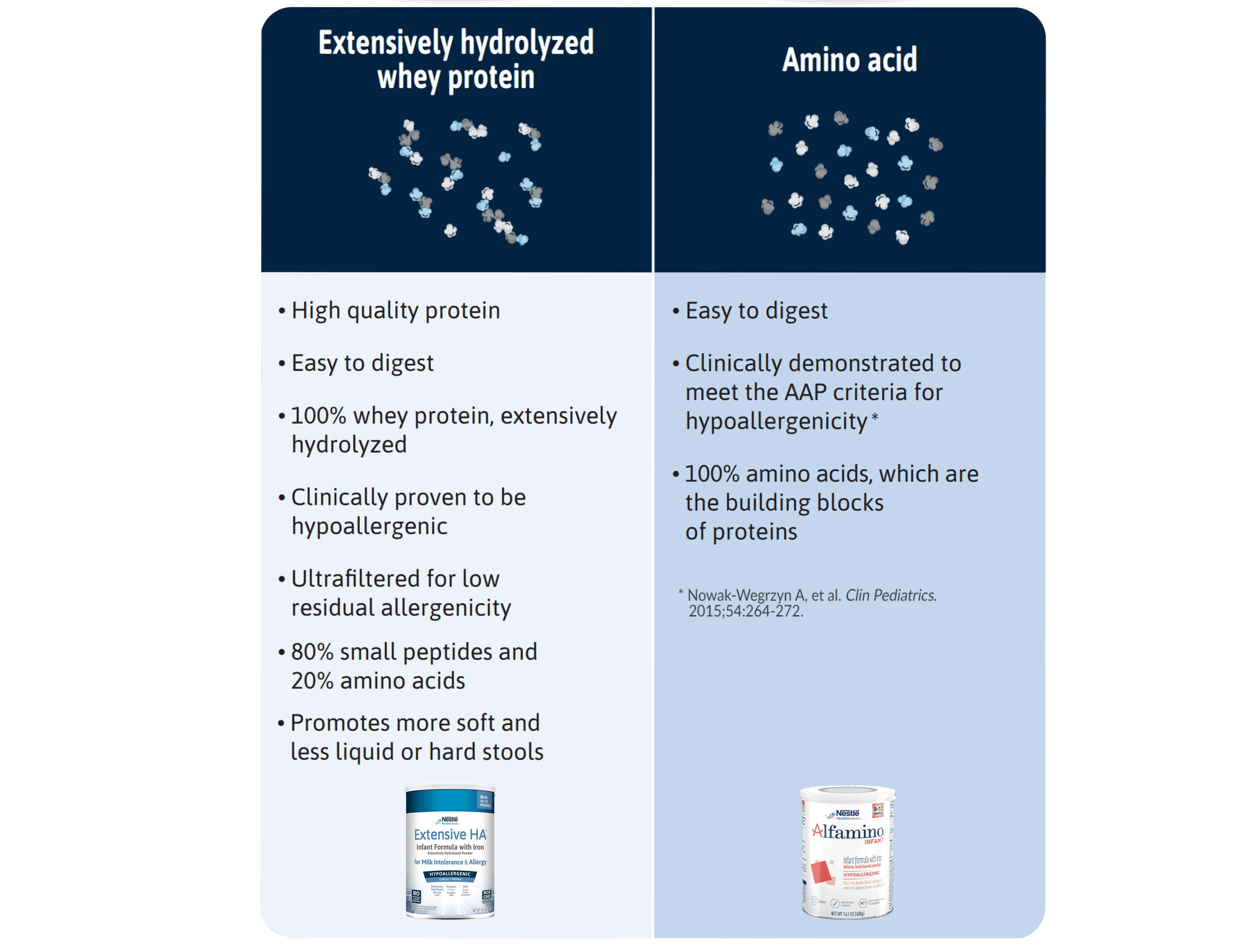
Breastfeeding mothers should eliminate milk and milk products from their own diet. For infants that are not breastfed, experts recommend feeding a hypoallergenic formula, such as an extensively hydrolyzed formula; however, in infants with severe or life-threatening symptoms or for those with multiple food allergies, an amino acid-based formula may be considered.
EoE is a chronic allergic disorder characterized by esophageal dysfunction and inflammation. Dietary elimination therapy has been shown to be an effective, drug-free prescription for the treatment of EoE.
EoE is linked to immune hypersensitivity to food. In EoE, large numbers of white blood cells called eosinophils are found in the tissue of the esophagus, whereas normally there are no eosinophils in the esophagus.
EoE can occur at any age, and the symptoms vary with age. Infants and toddlers may refuse food, or are not growing properly. School-age children often have recurring abdominal pain, trouble swallowing or are frequently vomiting. The esophagus can narrow to the point that food gets stuck; this is called food impaction and is a medical emergency. A major symptom with EoE is dysphagia due to the inflammation in esophagus. Adverse immune responses to food are the main cause of EoE in a large number of patients.
The relationship between food allergy and EoE is complex. In EoE, since the reactions are slower it is more difficult to establish the role of foods, and single foods are hard to pinpoint as the trigger.
One of the dietary regimens shown to be effective in EoE is the strict use of an amino acid-based formula.2,3 ACG recognizes the use of an amino acid-based diet as effective dietary management for eosinophilic GI disorders.4
The elemental diet (ED) is a diet therapy commonly used for EoE, and consists of an amino acid-based formula, free from intact proteins or peptides. Major allergy and gastroenterology societies suggest the use of an amino acid-based formula over an extensively hydrolyzed formula for the management of an ED. ED therapy may require nasogastric or gastrostomy tube feedings to achieve formula intake goals to meet nutritional needs.5
Food protein-induced enterocolitis syndrome (FPIES), is a non-IgE food allergy affecting the GI tract. FPIES is unlike typical food allergies, because symptoms (such as hives, swelling and wheezing) may not be immediate and do not show up on standard allergy tests. It is a condition causing severe vomiting and diarrhea. In some cases, symptoms can progress to dehydration and shock brought on by low blood pressure and poor blood circulation. The chronic reaction pattern includes increasingly severe vomiting, diarrhea and poor growth, possibly progressing to an illness mimicking a severe total-body infection.
Much like other food allergies, FPIES allergic reactions are triggered by ingesting a food allergen. Although any food can be a trigger, the most common culprits include milk, soy and grains. Most children with FPIES have only one or two food triggers, but it is possible to have FPIES reactions to multiple foods. FPIES often develops in infancy, usually when a baby is introduced to solid food or formula.
The best way to manage FPIES is to strictly avoid the food that triggers an allergic response. ESPGHAN guidelines recommend the use of an amino-acid-based formula for the management of FPIES, particularly if in association with growth faltering.6,7 Variety and dietary advancement is vital to an infant’s nutrition and development and can be challenging in infants with multiple food FPIES or feeding issues. FPIES patients should be monitored regularly for the development of tolerance and foods should be introduced using physician-supervised challenges.8
The Importance of Nutritional Support
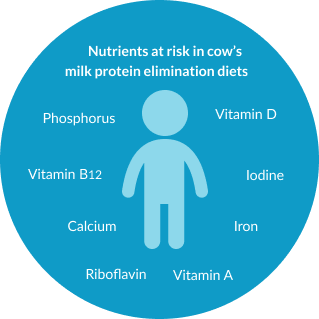
Without dietetic support, children with CMPA and/or multiple food allergies or EoE are at an increased risk of nutritional deficiencies,9 which can lead to significantly lower growth parameters.10
Therefore, as infants with food allergies start complementary feeding, continued dietetic support is important as it can be challenging for caregivers to provide an appropriate elimination diet which ensures a sufficient energy and nutrient intake.11
Food Allergy Or Non-Allergic Food Hypersensitivity
Non-allergic food hypersensitivities, such as intolerances, result from the inability to digest certain components of foods, i.e. lactose or fructose, or, less commonly, food colouring, additives or preservatives. Non-allergic food hypersensitivities do not involve the immune system and are much more common than food allergies.
Food allergies arise through an immunological reaction to certain allergens in food. These allergens are almost always proteins. Other components in food, such as lactose and other carbohydrates, do not commonly act as allergens. Certain food protein allergens cause more or more severe reactions than others.
Here are nine most common allergens accounting for approximately 90 percent of all allergic reactions to food in children.
Our Range of Tailor-Made Nutritional Solutions
Successful management of a pediatric food allergy, like CMPA, starts with an early diagnosis and requires ongoing support to ensure that infants and young children receive an appropriate elimination diet in order to reach their full potential. Nestlé Health Science is committed to helping you and your patients throughout the diagnosis and management journey.
There are several types of hypoallergenic formulas, including Extensively Hydrolyzed Formulas (EHF) and Amino Acid-Based Formulas.
Support Resources
You must be logged in to view all resources.
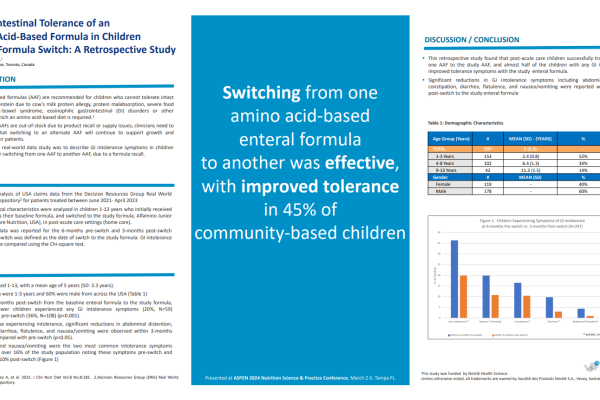
14 Evidence Found
29 Tools and Product Support Found
2 Patient Resources Found
30 Videos
References
1. Koletzko S, et al. Diagnostic Approach and Management of Cow’s-Milk Protein Allergy in Infants and Children: ESPGHAN GI Committee Practical Guidelines. J Pediatr Gastroenterol Nutr 2012;55(2):221-229.
2. Henderson CJ et al. Comparative Dietary Therapy Effectiveness in Remission of Pediatric Eosinophilic Esophagitis. J Allergy Clin Immunol 2012; 129(6): 1570–1578.
3. Greenhawt M et al. The Management of Eosinophilic Esophagitis. The Journal of Allergy and Clinical Immunology: In Practice 2013;1(4):332-340.
4. Dellon ES et al. ACG clinical guideline: Evidence-based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (EoE). Am J Gastroenterol. 2013;108:679-692.
5. Groetch, M et al. Dietary Therapy and Nutrition Management of Eosinophilic Esophagitis: A Work Group Report of the American Academy of Allergy, Asthma, and Immunology. J Allergy Clin Immunol Pract 2017;5(2):312-24)
6. Venter C, Groetch M. Nutritional management of food protein-induced enterocolitis syndrome. Curr Opin Allergy Clin Immunol 2014 Jun;14(3):255-262.
7. Koletzko S et al. Diagnostic approach and management of cow’s‐milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines. J Pediatr Gastroenterol Nutr. 2012;55:221-229.
8. Leonard et al. Food protein-induced enterocolitis syndrome: a review of the new guidelines World Allergy Organization Journal (2018) 11:4.
9. ASCIA 2017 – Food Allergy Clinical Update for Dietitians. Received from https://etrainingdiet.ascia.org.au/login/index.php on 5th June 2019.
10. Robbins et al. Milk allergy is associated with decreased growth in U.S. children. J Allergy Clin Immunol. 2014 December; 134(6):1466-1468.
11. Meyer, R. Nutritional disorders resulting from food allergy in children. Pediatr Allergy Immunol. 2018; 29:689–704.