About Impaired GI Function
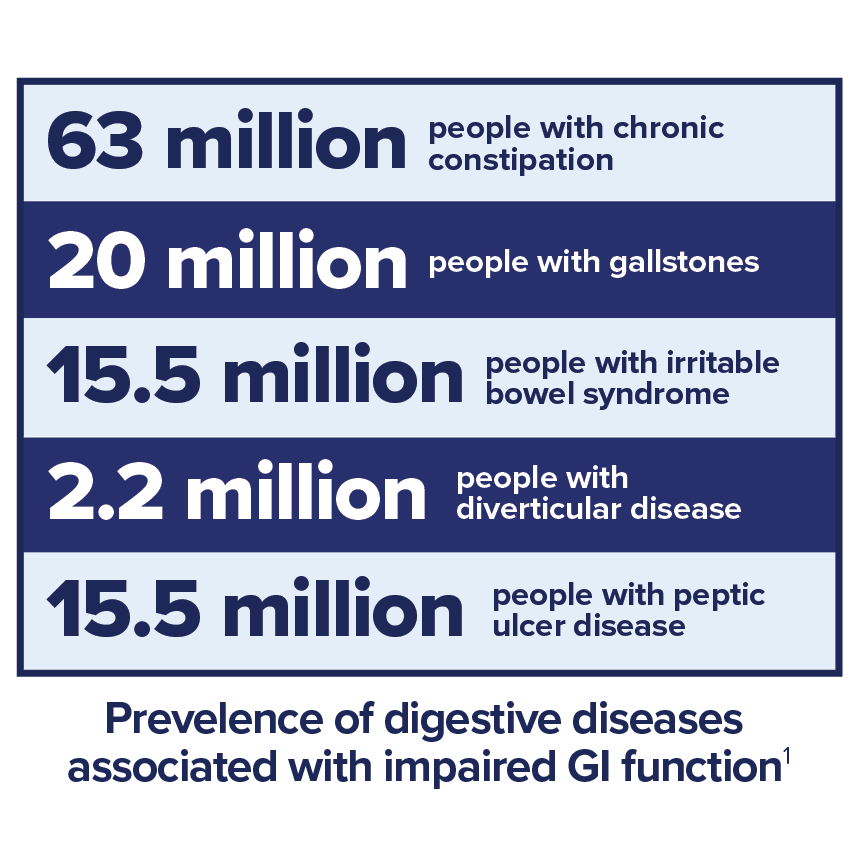
Digestive diseases can negatively impact an adult’s gastrointestinal (GI) function. Between 60-70 million Americans are affected by digestive diseases, resulting in 21.7 million hospitalizations per year. 1
Impaired GI function impedes the normal digestive process, leading to potential discomfort such as pain, bloating, nausea, diarrhea, and various other symptoms that can significantly diminish an individual's quality of life.
There are many ways in which GI impairment can present in an adult patient. Among the most common include:
- Gut motility issues that may lead to abdominal pain, constipation and/or diarrhea
- Digestive tract inflammation resulting in malabsorption
- Structural abnormalities that may affect nutrient digestion and absorption
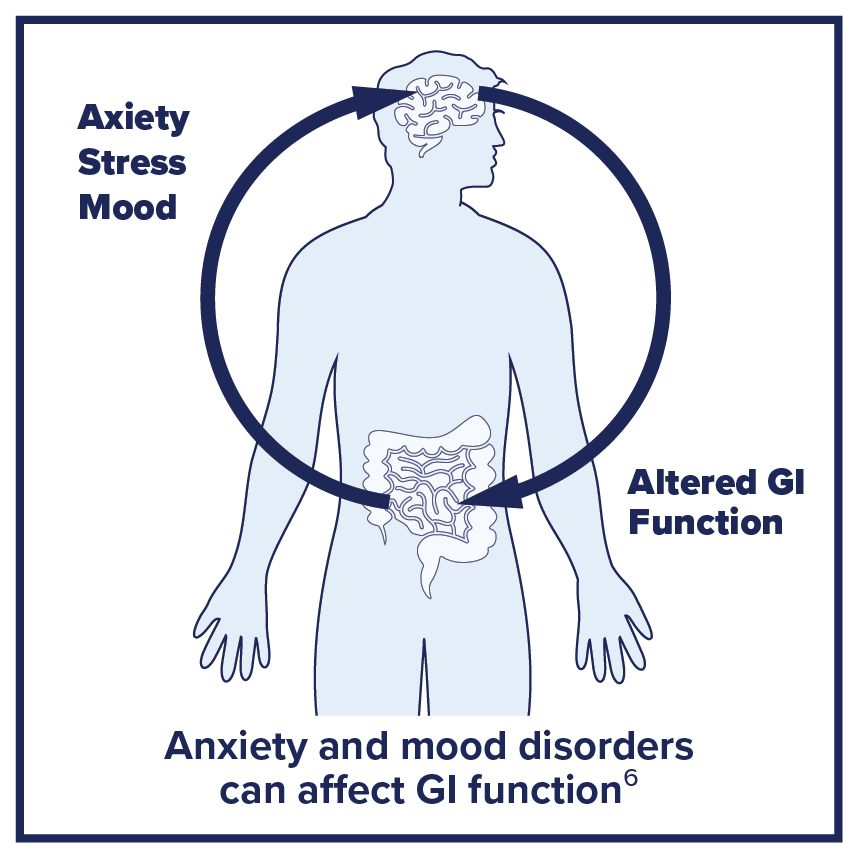
Emerging research on the gut-brain axis suggests that neuronal changes due to anxiety and mood disorders can also alter GI function by affecting the gut microbiota and resulting in symptoms of GI distress.7
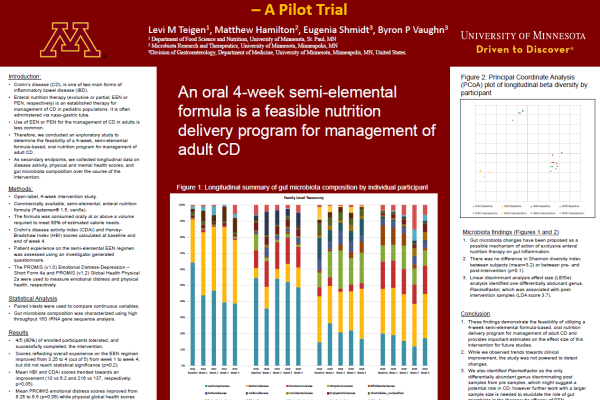
GI impairment is often linked to a chronic GI-related illness, such as Crohn’s disease or celiac disease, but it can also happen under acute conditions, including during critical illness, pancreatitis, in periods of antibiotic use or while undergoing cancer treatment.5,6
While impaired GI function in adults can be related to a diagnosed digestive disorder, it can also serve as a symptom of an underlying condition or coexisting comorbidities. Functional and motility disorders of the GI tract may also lead to intolerance and inadequate nutritional intake. Working as a multidisciplinary team to normalize a patient’s nutritional status can go a long way toward helping them heal and/or manage their other conditions.8
Nutrition & Impaired GI Function
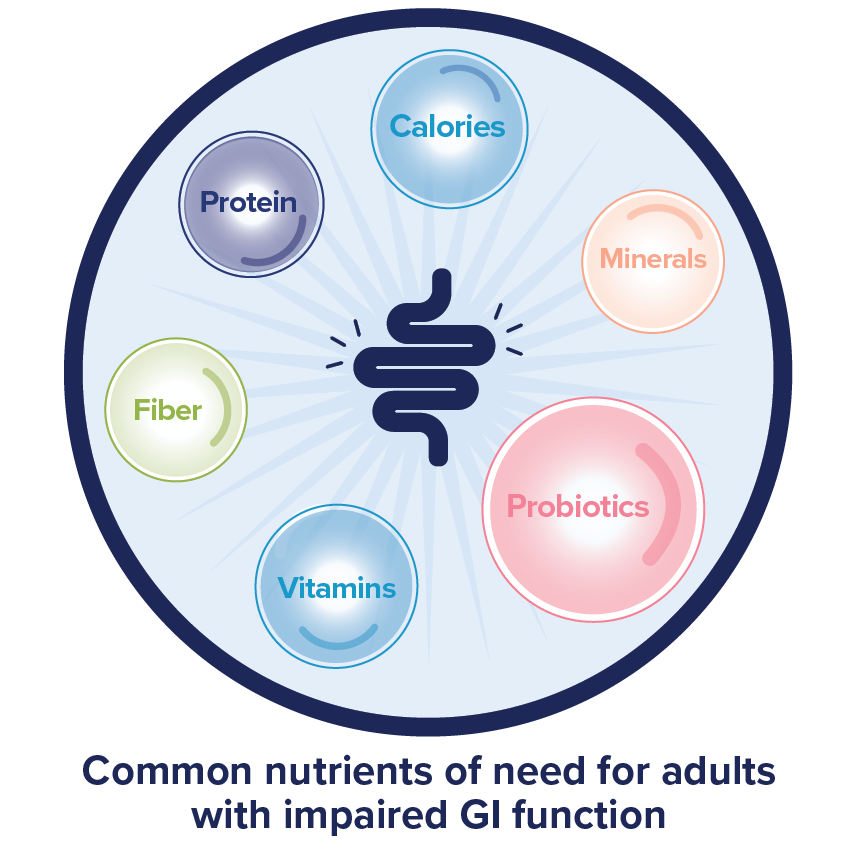
Because nutrient intake and absorption can be compromised in cases of adult GI impairment, the use of enteral nutrition or oral nutrition supplements may be required as a supplement to the diet or to meet all of a patient’s complete nutrition needs.
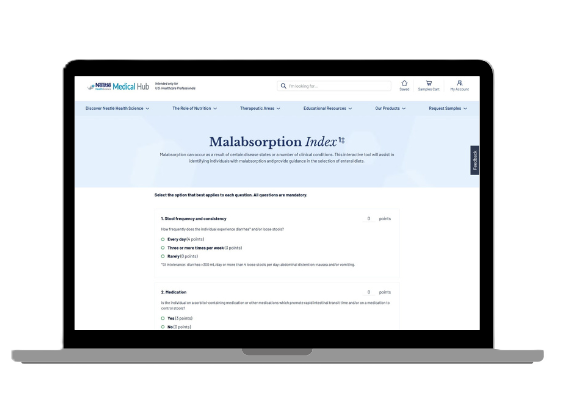
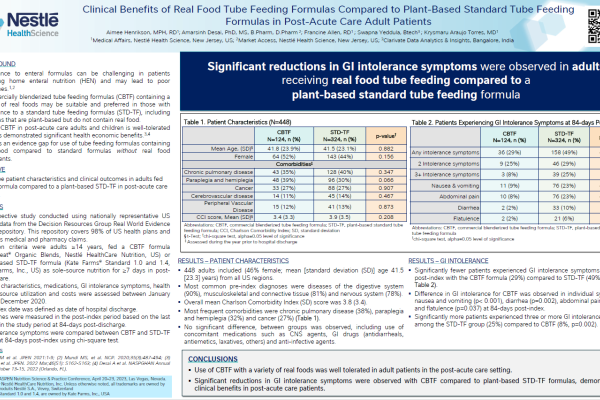
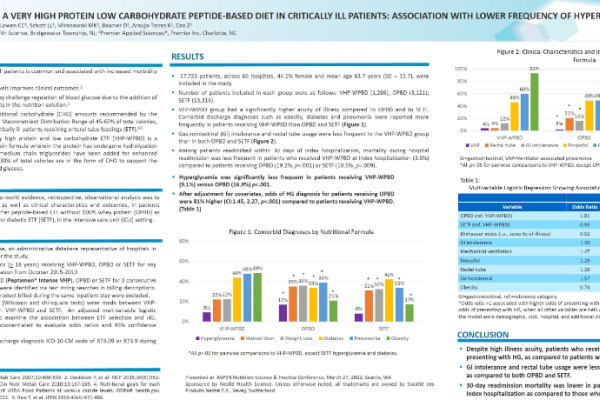
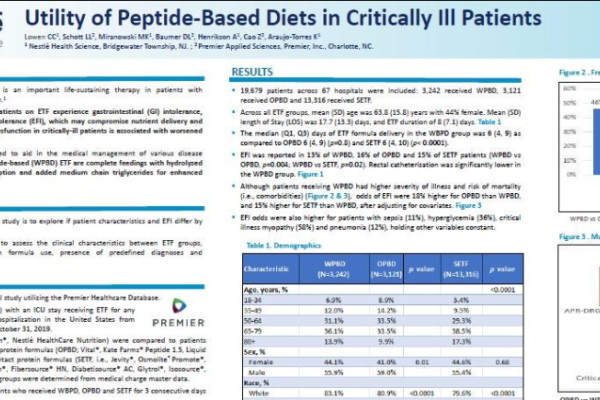
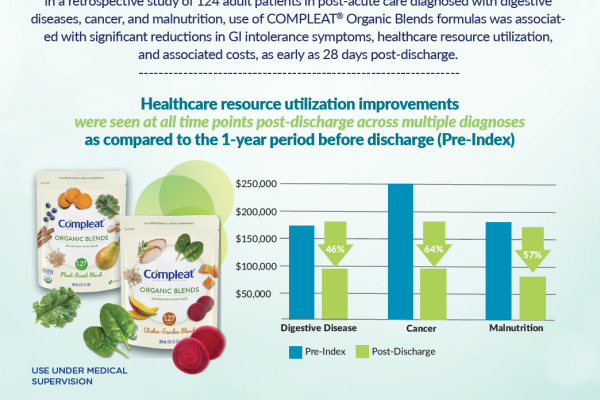
Insufficient intake and malabsorption of calories and protein are among the most serious consequences of impaired GI function in adults and can affect a patient’s health and quality of life. Micronutrient deficiencies are also common in adults with impaired GI function, particularly iron, zinc, vitamin B12 and vitamin D. The consumption of specialized formulas containing hydrolyzed high-quality 100% whey protein, medium-chain triglycerides, vitamins, and minerals has been shown to offer potential benefits, including improved GI tolerance, tissue repair, and healing.6,10,11 Blenderized whole food formulas have also shown improvement in GI tolerance.
No matter the cause of GI impairment in adults, it is incumbent on the nutritional support team to find a solution that is well tolerated by the patient, addresses nutrition intake gaps and puts the patient on a path toward healing.10 Oral or enteral nutrition treatments are preferred if the digestive system can tolerate this form of nutrition, while parenteral nutrition should only be used in the most severe cases as it is associated with greater complications.8
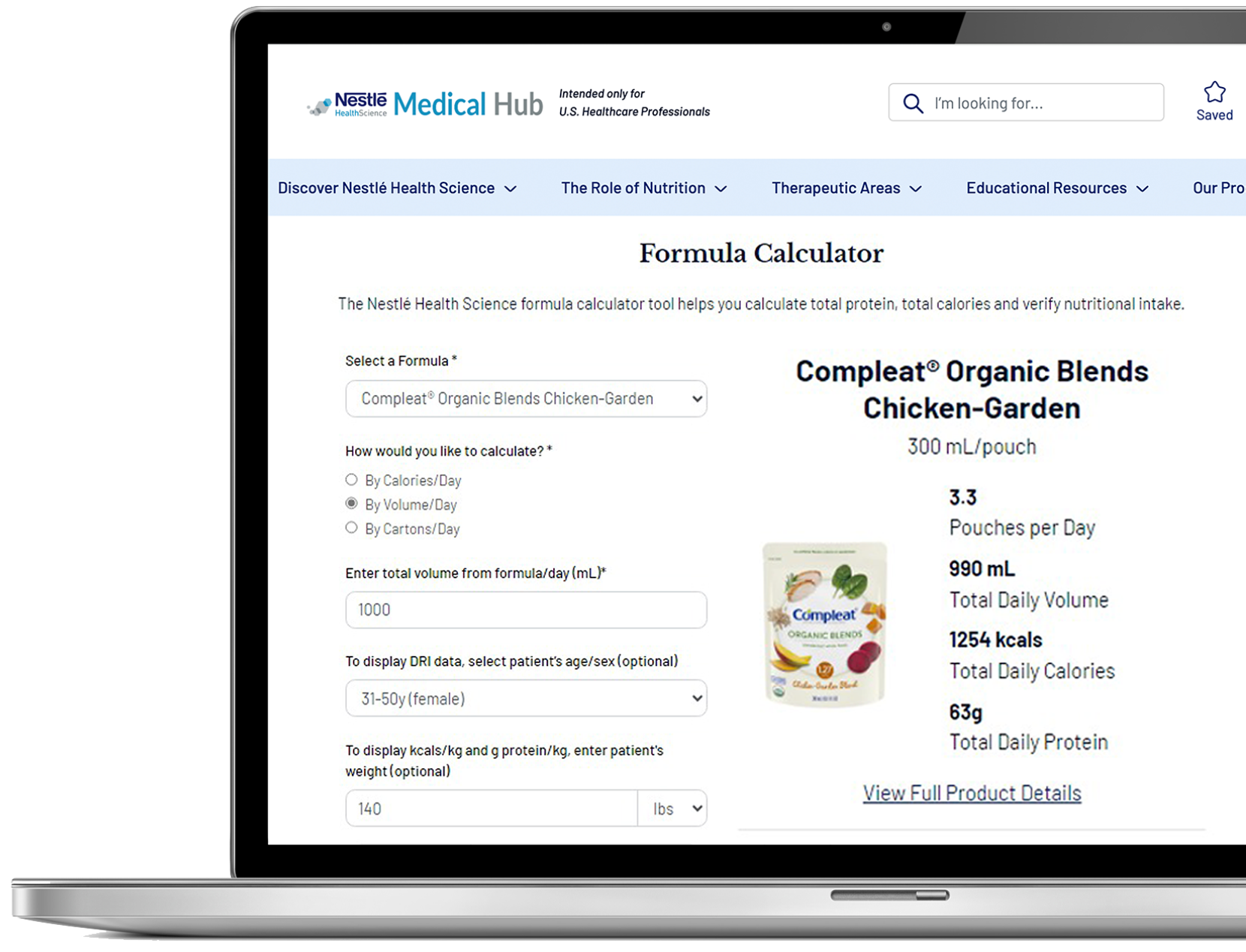
Nestlé Health Science offers a diverse range of enteral and oral nutrition solutions specifically designed to assist adults with impaired GI function. These solutions aim to address nutrient deficiencies, prevent weight loss, and combat malnutrition resulting from inadequate nutrient intake. Our specialized GI formulas have undergone thorough clinical testing and are backed by extensive research, instilling healthcare practitioners with the confidence to incorporate them into treatment plans. Moreover, we offer a wide variety of flavors and recipes to cater to diverse tastes, effectively preventing the occasional monotony associated with specialized nutrition therapy.
Support Resources
You must be logged in to view all resources.
27 Evidence Found
23 Tools and Product Support Found
31 Videos
References
- National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Digestive Diseases Statistics for the United States. https://www.niddk.nih.gov/health-information/health-statistics/digestive-diseases Last reviewed November 2014.
- Farré R, Fiorani M, Rahiman SA, Gianluca M. Intestinal permeability, inflammation and the role of nutrients. Nutrients. 2020;12,1185. Doi:10.3390/nu12041185. https://pubmed.ncbi.nlm.nih.gov/32340206/
- Reintam Blaser A, Preiser JC, Fruhwald S, et al. Gastrointestinal dysfunction in the critically ill: a systematic scoping review and research agenda proposed by the Section of Metabolism, Endocrinology and Nutrition of the European Society of Intensive Care Medicine. Crit Care. 2020. 24: 224. https://doi.org/10.1186/s13054-020-02889-4.
- Spiegel BMR, Khanna D, Bolus R, et al. Understanding gastrointestinal distress: a framework for clinical practice. Am J Gastroenterol. 2011;106(3):380-385. DOI: 10.1038/ajg.2010.383 https://journals.lww.com/ajg/abstract/2011/03000/understanding_gastrointestinal_distress__a.1.aspx
- Gastrointestinal Complications (PDQ®)–Health Professional Version, National Cancer Institute. Updated May 9, 2023. https://www.cancer.gov/about-cancer/treatment/side-effects/constipation/gi-complications-hp-pdq
- Mohamed Elfadil O, Shah RN, Hurt RT, Mundi MS. Peptide-based formula: Clinical applications and benefits. Nutr Clin Pract. 2023 Apr;38(2):318-328. doi: 10.1002/ncp.10961. Epub 2023 Feb 21. PMID: 36802281. https://aspenjournals.onlinelibrary.wiley.com/doi/10.1002/ncp.10961
- Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015 Apr-Jun;28(2):203-209. PMID: 25830558; PMCID: PMC4367209.
- Nightingale JMD, Paine P, McLaughlin J on behalf of the Small Bowel and Nutrition Committee and the Neurogastroenterology and Motility Committee of the British Society of Gastroenterology, et al The management of adult patients with severe chronic small intestinal dysmotility Gut 2020;69:2074-2092. https://gut.bmj.com/content/69/12/2074
- Samuel J (2022) Brief Note on Functional and Structural Gastrointestinal Disorder. J Hepatol Gastroint Dis. 8:203. https://www.longdom.org/open-access/brief-note-on-functional-and-structural-gastrointestinal-disorder-91249.html
- Berger MM, Hurni CA. Management of gastrointestinal failure in the adult critical care setting. Curr Opin Crit Care. 2022 Apr 1;28(2):190-197. doi: 10.1097/MCC.0000000000000924. PMID: 35131994; PMCID: PMC9990607.
- Abrahão V. Nourishing the dysfunctional gut and whey protein. Curr Opin Clin Nutr Metab Care. 2012 Sep;15(5):480-4. doi: 10.1097/MCO.0b013e328356b71e. PMID: 22878241.