Malnutrition
Impact on Outcomes and Cost of Care
Malnutrition increases morbidity, hospital admissions, infections, and pressure injuries, contributing to an estimated annual cost of disease associated malnutrition in the United States of more than $156 Billion.1-4
Intervention with specialized nutrition may lower overall cost of care, improve satisfaction and achieve better outcomes in patients with, or at risk of, malnutrition.5-7
Value of Nutrition Intervention
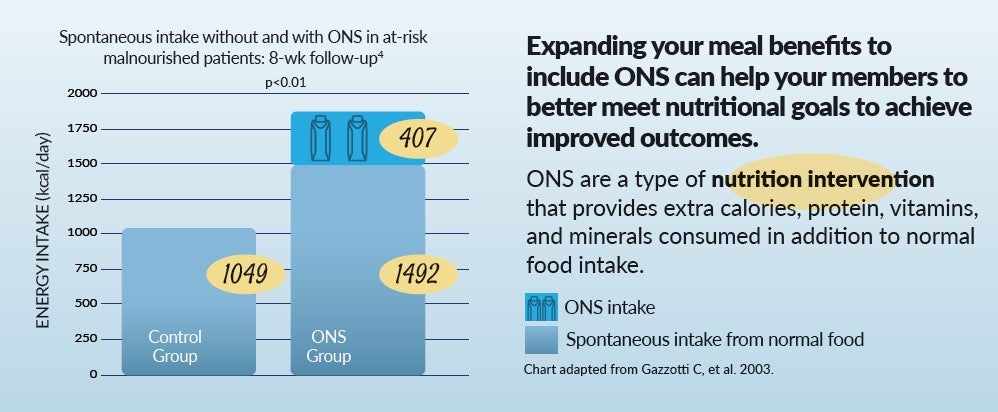
Oral Nutrition Supplements, or ONS, are a type of nutrition intervention providing extra calories, protein, vitamins and minerals consumed in addition to normal food intake.
In patients with, or at risk of, malnutrition adding ONS has been associated with:
- 21% reduction in length of stay (LOS) and a 21.6% decline in episode cost in hospitalized adults8
- 35% reduction in complications in surgical patients9
- 26% reduction in 30-day readmission rates in adults6
Clinically demonstrated in multiple patient populations across the continuum of care:1-3,16,20-32
- After hip fracture or other major orthopedic surgery
- Chronic lung disease
- Heart disease
- Wound care
- Chronic kidney disease/ESRD
- Oncology
- Community and home care
- Hospital at home
- Rehabilitation centers
- Ambulatory surgery centers
- Nursing homes
- Hospitals
Medicare Advantage Plans
What if with one simple, evidence-based change you could:10-13
- Lower overall cost of care
- Improve member satisfaction scores
- Retain & grow your Medicare Advantage base
- Achieve better outcomes than through food alone5,14-18
Enhancing nutritional intake with oral nutritional supplements (ONS) for chronically ill patients with (or at risk of) malnutrition along with regular meals has been shown to:
- Reduce risk of falls by 60%5
- Decrease 30-day hospital readmission rates by 26%6
- Reduce hospitalizations by 16.5%13-19
Mini Nutrition Assessment (MNA)® - Making the Link to Intervention Easier and Quicker
The MNA® is the most well-validated nutrition screening and assessment tool for patients age 65 and above who are malnourished or at risk of malnutrition. The MNA® consists of six questions and streamlines the screening process.
The recent enhancements of Medicare Advantage Special Supplemental Benefits for the Chronically Ill (SSBCI) allow you to expand benefits to include food, produce, and meals in your plans.
Expanding your meal benefits to include ONS can help your members to better meet nutritional goals to achieve improved outcomes.
Tools & Resources
Access Nestlé's evidence-based protocols, tools and products to help lower total cost of care and improve outcomes in members with malnutrition.
Contact Us
Contact Us now to learn more about reducing total cost of care and improving clinical outcomes with our expansive portfolio of nutrition products.
Please include your first and last name, email address, phone number, company, and title in your email.
References
1. Sorenson J et al. Clin Nutr. 2008;27:340-349.
2. Collins PF et al. Proc Nutr Soc. 2010;69(OCE2):E148.
3. Dreyfus J et al. Am J Med Qual. 2018;33:348-358.
4. Snider JT, et al. JPEN. 2014:38:77S-85S
5. Neelemaat F, et al. J Am Geriatric Soc 2012;60: 691-699.
6. Sriram K, et al JPEN 2017; 41:384-391.
7. Elia M, et al. Clin Nutr 28. Philipson TJ et al. Am J Manag Care. 2013;19:121-128.
8. Philipson TJ et al. Am J Manag Care. 2013;19:121-128
9. Elia M et al. Clin Nutr. 2016;35:370-380.
10. Sulo S et al. Am Health Drug Benefits. 2017;10:262-270.
11. Philipson TJ et al. Am J Manag Care. 2013;19:121-128.
12. Elia M et al. Clin Nutr. 2016;35:125-137.
13. Arnaud-Battandier F et al. Clin Nutr. 2004;23:1096-1103
14. Cawood AL et al. Ageing Res Rev. 2012;11:278-296
15. Persson M et al. Clin Nutr. 2007;26:216-224.
16. Rabadi MH et al. Neurology. 2008;71:1856-1861.
17. Norman K et al. Clin Nutr. 2008;27:48-56.
18. Chapman IM et al. Am J Clin Nutr. 2009;89:880-889.
19. Elia M, et al. Clin Nutr 2016;35:125-137.
20. Beattie AH, et al. Gut 2000; 46:813-818.
21. Lawson RM, et al. Clin Nutr 2003;22:39-46.
22. Volkert D et al. Clin Nutr. 2018.
23. Myint MWW et al. Age Ageing. 2013;42:39-45.
24. Tyler R, et al. JPEN J Parenter Enteral Nutr. 2020;44(3):395-406.
25. Yeung SE, et al. Am J Clin Nutr. 2017;106(1):44-51.
26. Wang G, et al. Nutrients. 2015.7(6):4308-17.
27. Paccagnella A, et al. Support Care Cancer 2010;18:837-45.
28. Sanchez-Lara K, et al. Clin Nutr. 2014 Dec;33(6):1017-23.
29. Sezer S, et al. JPEN J Parenter Enteral Nutr. 2014 Nov;38(8): 960–965.
30. Huang, WJ, et al. J Nutr Health Aging. 2022; 26: 723–731.
31. Rozentryt, P, et al. J Cachexia Sarcopenia Muscle. 2010; 1: 35–42.
32. Kaiser MJ et al. J Am Ger Soc. 2010; 58:1734-1738.